Abstract
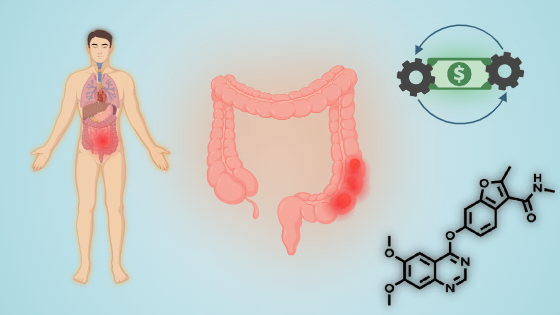
Background: Colorectal cancer, one of the most prevalent cancers globally, originates from polyps in the colon or rectum, which can develop into cancer over time. It remains a leading cause of cancer-related deaths, imposing significant economic and healthcare burdens. As the incidence of colorectal cancer continues to rise, particularly in developing healthcare systems, understanding the economic impact of treatment options is critical for informing clinical decisions and shaping healthcare policies.
Methods: Following PRISMA guidelines, an extensive literature search was conducted through databases including PubMed, Embase, and Scopus up to 7 October 2024. The inclusion criteria targeted studies utilizing cost-effectiveness analysis frameworks like Markov and Partitioned-Survival models, comparing fruquintinib to other cancer treatments. Key outcome measures focused on Incremental Cost-Effectiveness Ratios and Quality-Adjusted Life Years.
Results: Of the 49 articles screened, seven studies were eligible for inclusion. These studies provided a detailed economic evaluation of Fruquintinib against Regorafenib, placebo, and best supportive care. Notably, Fruquintinib was cost-effective in the Chinese healthcare setting with an ICER of $26,508 per QALY compared to $35,607 for Regorafenib. However, it did not meet cost-effectiveness thresholds when compared with placebo, with an ICER exceeding three times the GDP per capita in China, reflecting the economic challenges of implementing new cancer treatments.
Conclusion: Fruquintinib shows promise as a cost-effective treatment for metastatic colorectal cancer, particularly in healthcare settings like China, providing significant QALY gains compared to traditional therapies. However, its adoption is highly dependent on local economic thresholds and healthcare systems. While this study underscores the need to integrate economic and clinical outcomes in cancer treatment decisions, the drug's approval and data are currently limited to China, making it difficult to conclude its cost-effectiveness globally
Keywords:
Chronic kidney disease, Human deficiency virus, Systematic review, Meta-analysis, PLHIVReferences
1. Colorectal Cancer: WHO; 2023 [Available from: https://www.who.int/news-room/fact-sheets/detail/colorectal-cancer.
2. Hossain MS, Karuniawati H, Jairoun AA, Urbi Z, Ooi J, John A, et al. Colorectal Cancer: A Review of Carcinogenesis, Global Epidemiology, Current Challenges, Risk Factors, Preventive and Treatment Strategies. Cancers (Basel). 2022;14(7).
3. Salva de Torres C, Baraibar I, Saoudi González N, Ros J, Salva F, Rodríguez-Castells M, et al. Current and Emerging Treatment Paradigms in Colorectal Cancer: Integrating Hallmarks of Cancer. International Journal of Molecular Sciences. 2024;25(13):6967.
4. Gmeiner WH. Recent Advances in Therapeutic Strategies to Improve Colorectal Cancer Treatment. Cancers. 2024;16(5):1029.
5. Adebayo AS, Agbaje K, Adesina SK, Olajubutu O. Colorectal Cancer: Disease Process, Current Treatment Options, and Future Perspectives. Pharmaceutics. 2023;15(11):2620.
6. Lavacchi D, Roviello G, Guidolin A, Romano S, Venturini J, Caliman E, et al. Evaluation of Fruquintinib in the Continuum of Care of Patients with Colorectal Cancer. International Journal of Molecular Sciences. 2023;24(6):5840.
7. The Costs of Colorectal Cancer: American Cancer Society Cancer Action Network Available from: https://www.fightcancer.org/sites/default/files/national_documents/the-costs-of-colorectal-cancer.pdf.
8. Bhimani N, Wong GYM, Molloy C, Dieng M, Kelly PJ, Hugh TJ. Lifetime direct healthcare costs of treating colorectal cancer: a systematic review. The European Journal of Health Economics. 2023;24(4):513-37.
9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. bmj. 2021;372.
10. Thangamma Ag M, Vidyadharan B, Daniel RP, Sirur A, Kumar P, Thunga PG, et al. Cost and cost-effectiveness of treatments for rheumatic heart disease in low- and middle-income countries: a systematic review protocol. JBI Evid Synth. 2024;22(9):1886-97.
11. Mandrik OL, Severens JLH, Bardach A, Ghabri S, Hamel C, Mathes T, et al. Critical Appraisal of Systematic Reviews With Costs and Cost-Effectiveness Outcomes: An ISPOR Good Practices Task Force Report. Value Health. 2021;24(4):463-72.
12. Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. Bmj. 2020;368:l6890.
13. New cost-effectiveness updates from WHO-CHOICE: WHO; 2021 [Available from: https://www.who.int/news-room/feature-stories/detail/new-cost-effectiveness-updates-from-who-choice.
14. Cost-effectiveness analysis of later-line treatments for refractory metastatic colorectal cancer
Annual Meeting of the American Society of Clinical Oncology2024.
15. Guan X, Li H, Xiong X, Peng C, Wang N, Ma X, et al. Cost-effectiveness analysis of fruquintinib versus regorafenib as the third-line therapy for metastatic colorectal cancer in China. J Med Econ. 2021;24(1):339-44.
16. Huang Z, Zhou L, Zheng H, Zhan M. Cost-effectiveness analysis of fruquintinib in Chinese patients with refractory metastatic colorectal cancer. Int J Clin Pharm. 2024;46(4):872-80.
17. Obeng-Kusi M, Roe D, Erstad BL, Abraham I. Cost-effectiveness analysis of later-line therapies for metastatic colorectal cancer (mCRC) based on a novel methodology of network meta-analysis (NMA) of survival curves. Journal of Clinical Oncology. 2023;41(16_suppl):3605-.
18. Peng Z, Hou X, Huang Y, Xie T, Hua X. Cost-effectiveness analysis of fruquintinib for metastatic colorectal cancer third-line treatment in China. BMC Cancer. 2020;20(1):990.
19. Yao L, Han J, She L, Ding D, Liao M, Hu H, et al. Cost-effectiveness for metastatic colorectal cancer. Journal of Clinical Oncology. 2019;37(15_suppl):e15003-e.
20. Zhang PF, Xie D, Li Q. Cost-effectiveness analysis of fruquintinib as third-line treatment for patients with metastatic colorectal cancer. Tumori. 2020;106(5):400-5.
21. Kim DD. Developing Criteria for Health Economic Quality Evaluation Tool. Value in Health. 2023.
How to Cite
License
Copyright (c) 2025 Mona Thangamma AG , Shree Rath, Andria J N Sirur , Vijaya kumar Uthakalla, Santenna Chenchula , Swati Misra, Tuhin James Paulo , Debopriya, Chanchal Goyal , Ujjawal Sharma , G Vinod , Firdaus Samad, Arindam Biswas , Sree Sudha T Y

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright© by the author(s). Published by the Evidence Journals. This is an open access article distributed under the terms of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Most read articles by the same author(s)
- Ankita Gaonkar , Shree Rath, Rahini S, Manav Jain, Raman Swathy Vaman, Anindita Das , Samiya Manal, Divjot Singh Lamba, Purnoor Kaur , SUKRITI YADAV , Sanjev Dave , Ashlesha Ashok Tawde, Swati Misra, Sowmisri BM , Chanchal Goyal , Shreekant Bharti , Krishna Chaitanya Amerneni, Transforming medical diagnosis: a comprehensive review of AI and ML technologies , Evidence Public Health: Vol. 1 No. 1 (2025): JAN-MAR
- Aroop Mohanty, Priyadarshini. P, Sowntappan Balasubramanian , Santenna Chenchula, Ranjit Sah, Forecasting of Monkeypox Outbreak Trends in the most Affected Countries: A Join point regression modelling approach , Evidence Public Health: Vol. 1 No. 1 (2025): JAN-MAR