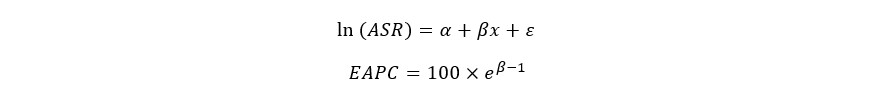
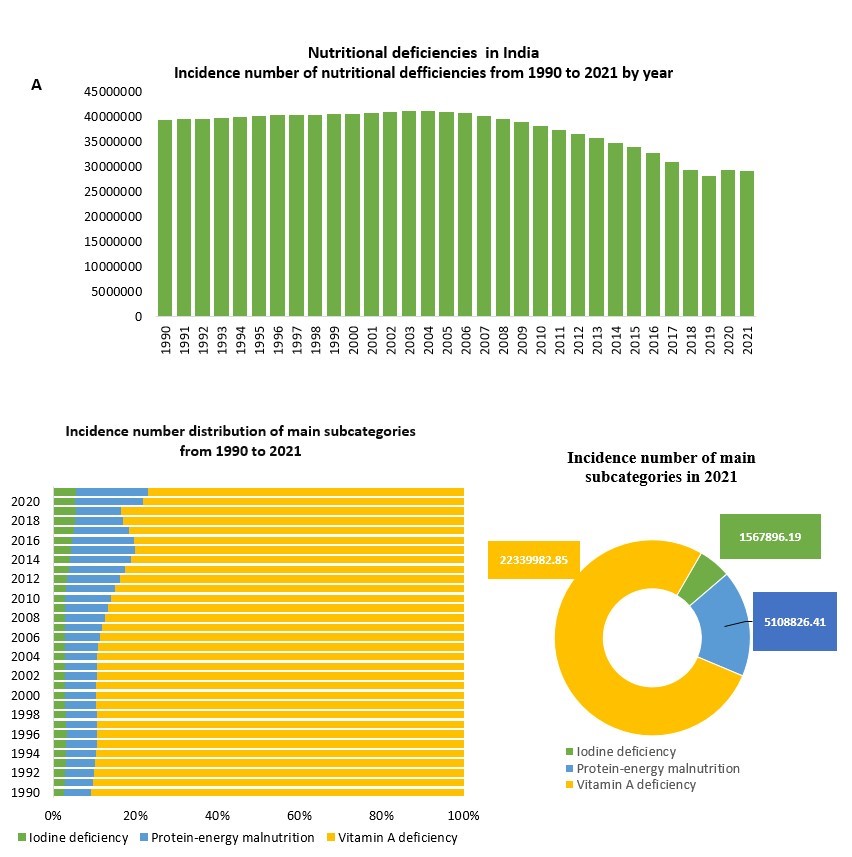
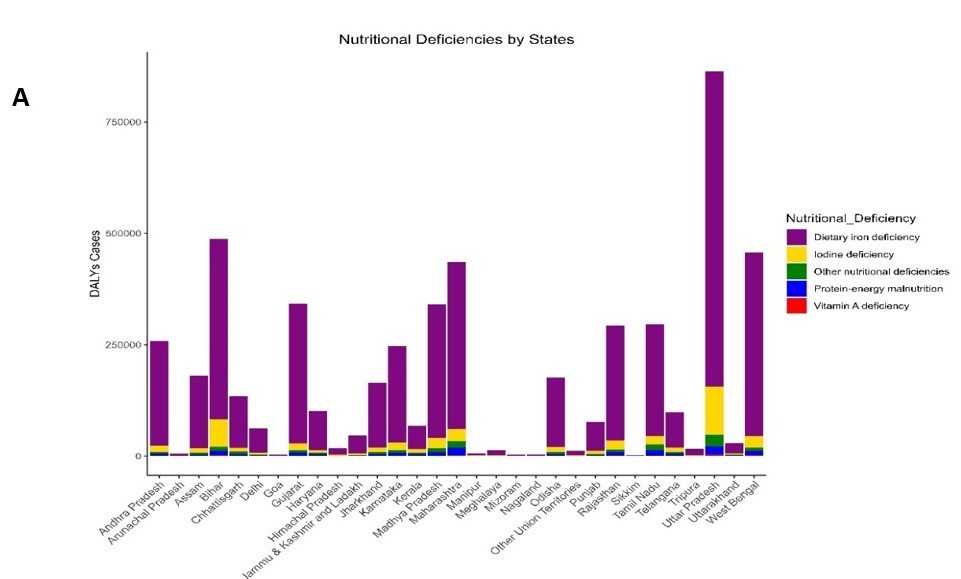
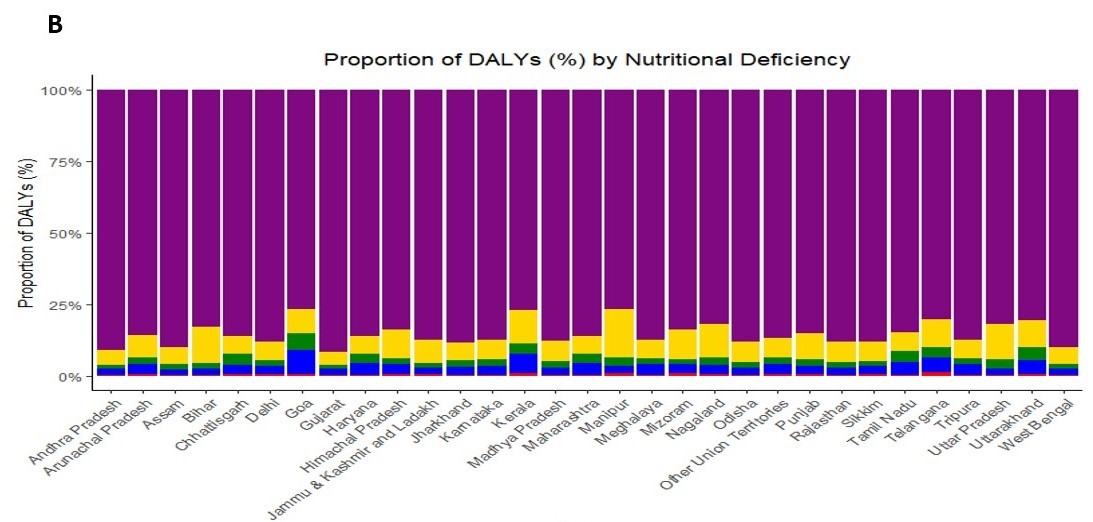
vitamin A and iodine deficiencies, which contribute to a range of adverse health outcomes, including anemia, stunting, and impaired cognitive development in children.
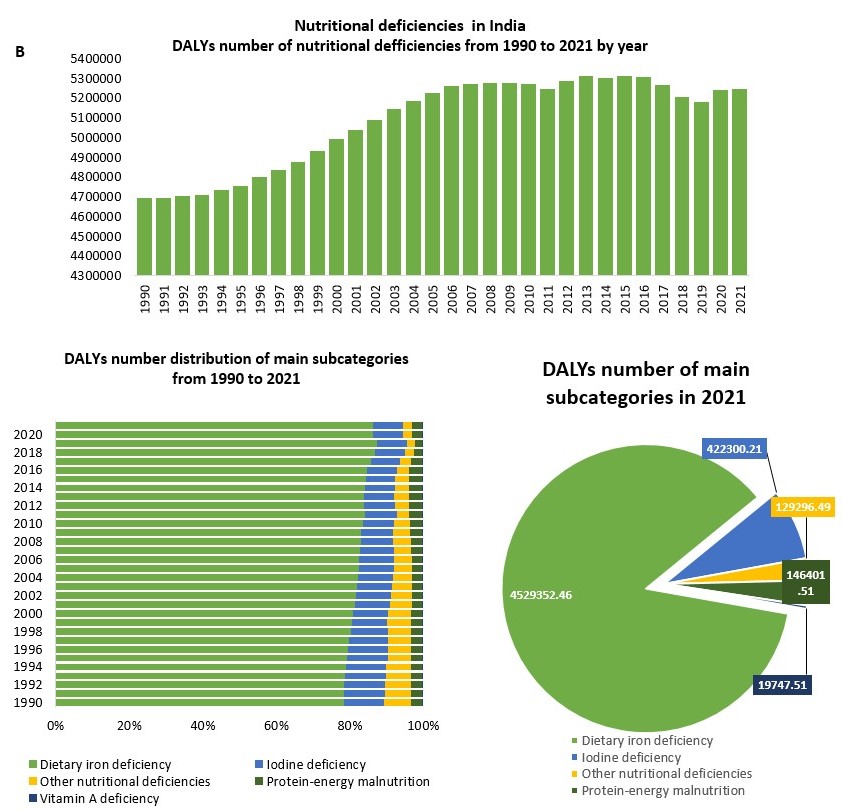
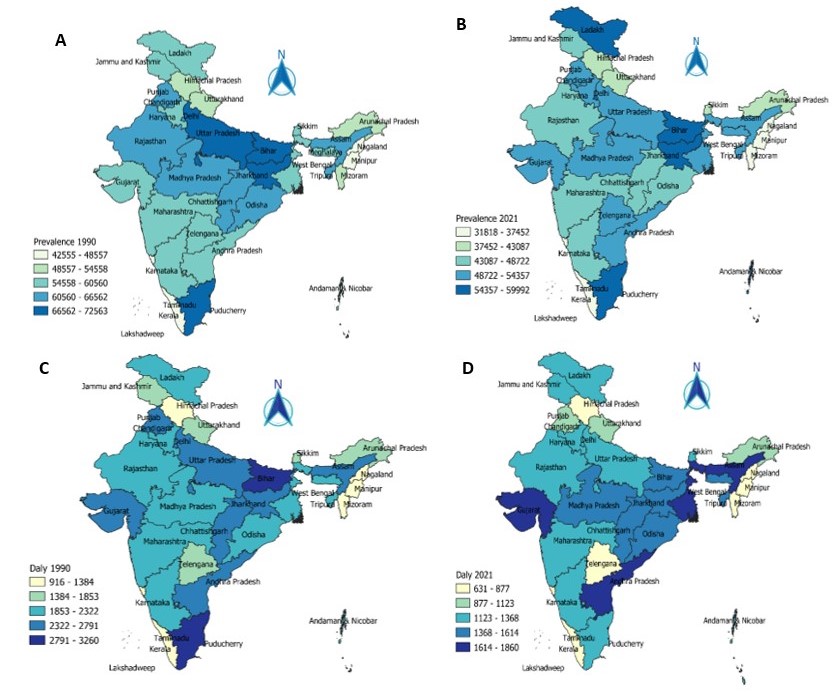
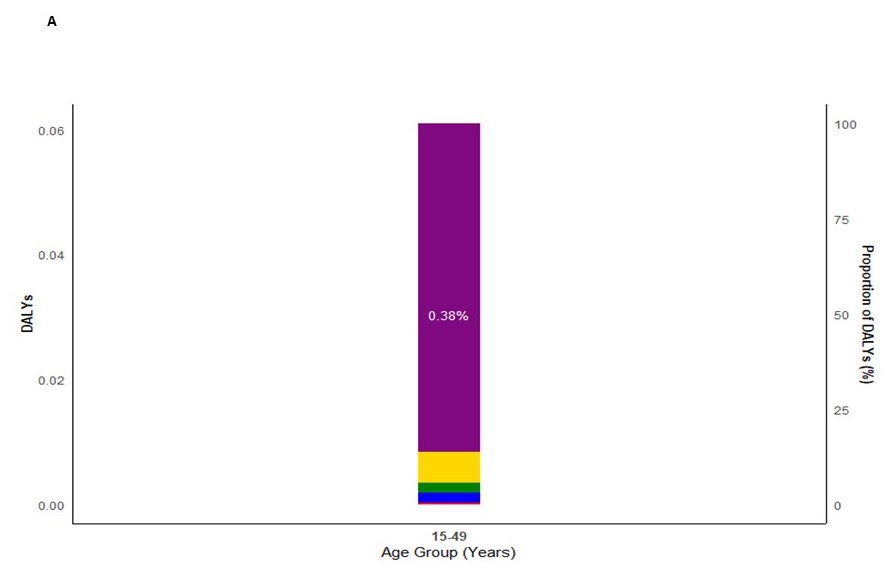
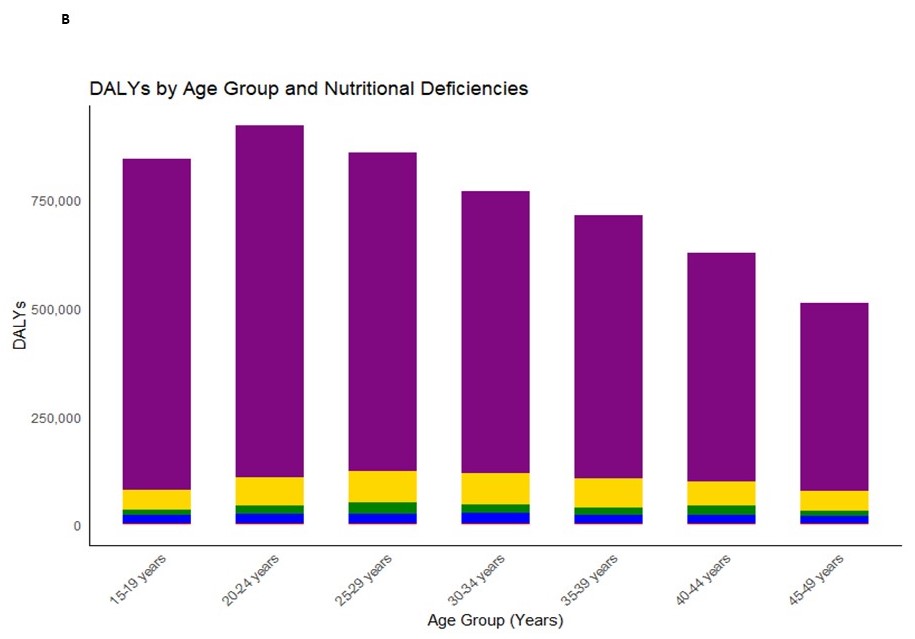
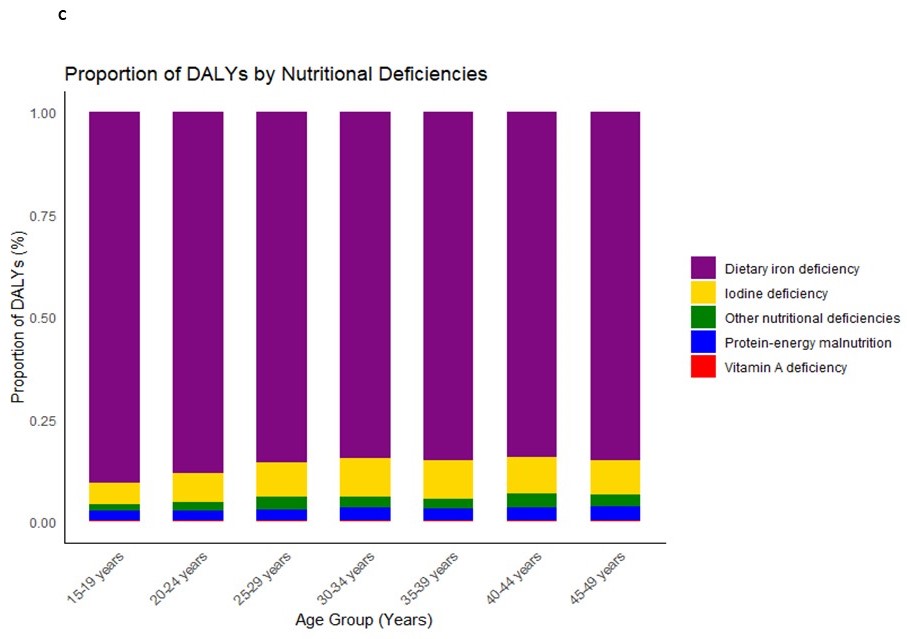
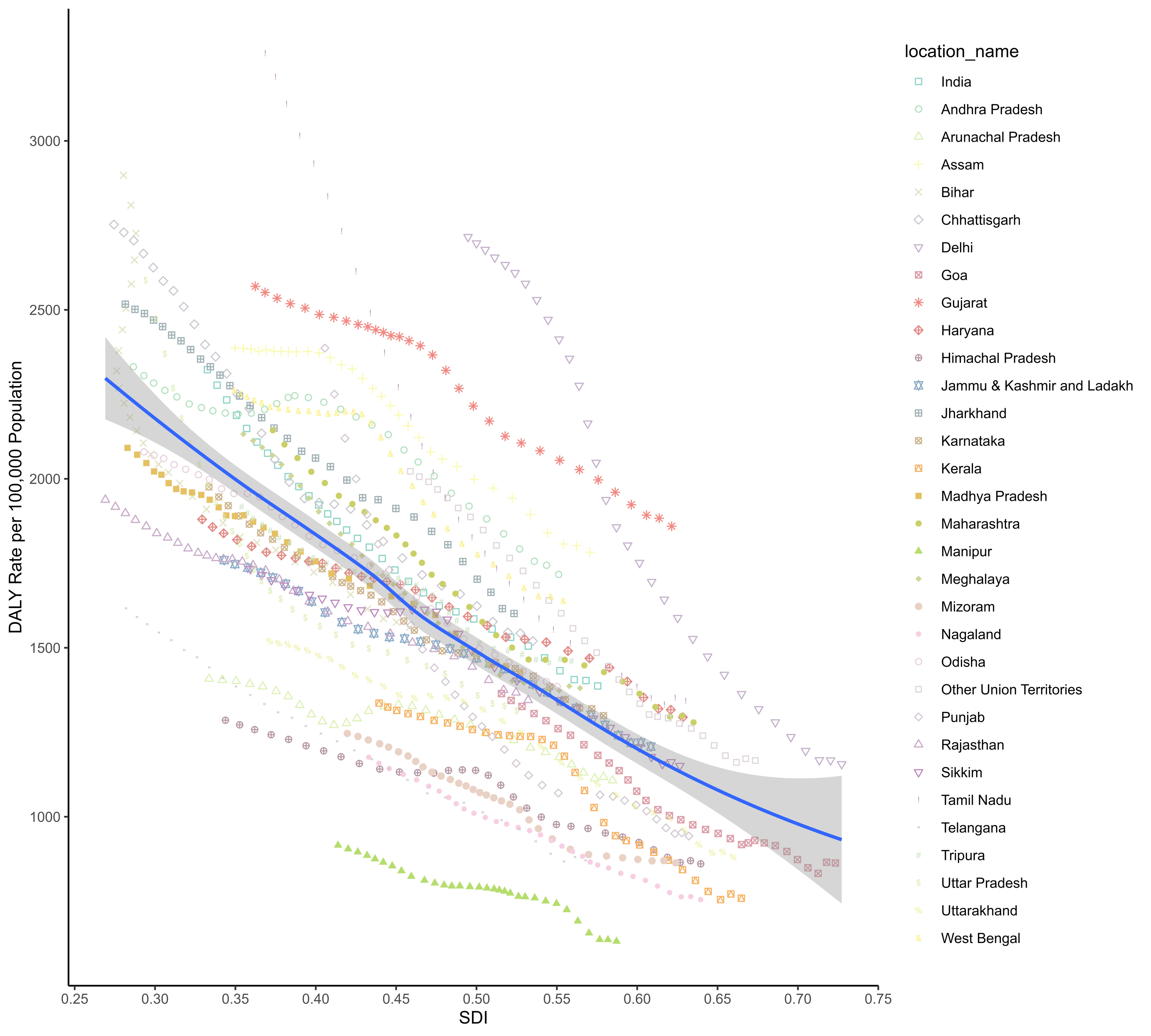
Nutritional deficiencies among reproductive-age women in India present a significant public health challenge, with anemia being one of the most prevalent issues. Anemia affects a substantial portion of this demographic, particularly pregnant and lactating women, due to inadequate dietary intake and high energy demands from work and childbearing responsibilities [1]. Malnutrition in India is multifaceted, encompassing undernutrition, micronutrient deficiencies, and overnutrition, with nearly one-third of women aged 15-49 years being underweight [2, 3]. The socio-economic factors contributing to these deficiencies include poverty, lack of education, and inadequate access to healthcare and nutrition services [2, 3]. Urban areas also exhibit significant nutritional disparities, with the poorest women experiencing higher rates of maternal thinness and anemia compared to their wealthier counterparts [4]. Despite India's economic growth, the distribution of resources remains uneven, exacerbating these nutritional challenges. The consequences of these deficiencies are profound, affecting women's reproductive health, economic productivity, and overall well-being [5]. Addressing these issues requires a multisectoral approach, including improved agricultural productivity, better food distribution systems, and enhanced public health initiatives focused on nutrition education and supplementation [3, 6]. Additionally, targeted interventions such as food fortification and the provision of iodized salt and iron supplements are crucial to mitigating these deficiencies and improving the health outcomes of women in this age group [6]. This study leverages data from the Global Burden of Disease (GBD) Study 2021 to estimate the burden and trends of nutritional deficiencies among reproductive-age women in India. The GBD database provides a comprehensive, age-standardized analysis of disease burden, offering valuable insights into temporal shifts in prevalence and associated disability-adjusted life years (DALYs) from 1990 to 2021. These trends are critical for understanding the evolving epidemiology of nutritional deficiencies in India, a country with diverse socio-economic and geographic contexts.
Despite improvements in nutrition and health interventions, such as fortified foods and maternal supplementation programs, the burden of nutritional deficiencies has remained stubbornly high. This study aims to provide evidence to inform policy, prioritize interventions, and drive progress towards achieving better health outcomes for women in India, with a focus on sustainable, long-term solutions. Additionally, this research directly contributes to Sustainable Development Goal 2 (SDG 2), specifically targeting the end of all forms of malnutrition by 2030, as outlined by the United Nations. It emphasizes the importance of tailored public health strategies to meet these global nutritional targets effectively.
Methods
Data source
The data analyzed and presented in this study comes from the GBD 2021 public datasets, which are accessible at (http://ghdx.healthdata.org/gbd-results/). The GBD 2021 study incorporates the most recent and comprehensive epidemiological data, applying standardized methods to assess the global burden of health loss and its associated risk factors for a wide range of diseases and conditions. It evaluates 358 causes of death, 364 causes of years lived with disability (YLDs), and 373 causes of DALYs across 204 countries and territories from 1990 to 2021. The GBD methodology integrates data from various sources, including national censuses, household surveys, civil registration and vital statistics, health service utilization data, disease registries, satellite imagery, and air pollution monitors. These datasets are harmonized using advanced statistical techniques to provide consistent and comparable estimates of health outcomes globally. Further details of the GBD 2021 methodology are available in the published literature [7].
Nutritional deficiencies were categorized according to the 10th revision of the International Classification of Diseases (ICD-10), with relevant codes including D50–D53.9, E00–E02, E40–E46.9, E50–E61.9, E63–E64.9, and Z13.2–Z13.3. These deficiencies were further classified into key subgroups: protein-energy malnutrition (E40–E46.9, E64.0), iodine deficiencies (E00–E02), vitamin A deficiency (E50–E50.9, E64.1), dietary iron deficiencies (D50–D50.9), and other nutrient deficiencies (D51–D53.9, E51–E61.9, E63–E64, E64.2–E64.9).